Building effective dyad growth teams
- Category: Physician Engagement, News
- Written By: Tim Hewitt

Google the term “physician-led/professionally managed” and you will see there are millions of results. The concept of bringing clinical and administrative leaders together has found its place in today’s healthcare vocabulary amid the consolidation, integration and assimilation of physician practices.
Yet medical group leaders know that it is counterproductive to pay lip service to the claim of being “physician-led/professionally managed.” In too many cases it is a nebulous ideal that is difficult to define and harder to achieve without the resources, structure and culture to fully engage the medical staff. Just as employment does not guarantee engagement, the major investments required to build an employed enterprise do not magically create loyalty, generate increased revenue or guarantee strategic growth.
Forming a dyad team management structure — consisting of a clinical member and an administrative member who co-lead or co-manage their area of responsibility — can be a step toward better organizational outcomes.
Engagement by the numbers
Industry data points to significant barriers due to wide gaps in communication, trust and collaboration between physicians and administrative leaders. According to an AthenaHealth/Epocrates survey, only 20% of physician respondents met the criteria for engagement. Low scores in “satisfaction with leadership” correlate with low levels of engagement.
Complicating the equation is the tendency for some administrators to overestimate their physicians’ engagement levels. Jackson Healthcare’s Physician Engagement survey identified significant gaps in what executives perceive versus what physicians report on the level of trust in leadership and involvement in decision-making. The survey also revealed a disheartening point of agreement: Both physicians and executives assigned equally low scores to the quality of communication across the organization.
Enemies of engagement: Lack of time, poor communication
These industry reports align with the perspectives of the practice managers and medical group executives who attended the MGMA 2016 Annual Conference session, “Building Effective Dyad Teams.” The session explored methods for engaging physicians with administrators in dyad teams and included an interactive poll, which made it clear that communication and time are the top barriers to achieving physician engagement.
 The challenges of communication and time are closely linked, said Shelly Phinney, MGMA member, process excellence facilitator, quality system office, Saint Luke’s Health System, Kansas City, Mo. Previously at Truman Medical Center Lakewood, Kansas City, Mo., Phinney worked for five years as the director of family medicine in the dyad team model with a physician who was the department chair.
The challenges of communication and time are closely linked, said Shelly Phinney, MGMA member, process excellence facilitator, quality system office, Saint Luke’s Health System, Kansas City, Mo. Previously at Truman Medical Center Lakewood, Kansas City, Mo., Phinney worked for five years as the director of family medicine in the dyad team model with a physician who was the department chair.
“We made it a priority to share our expectations and build lines of communication that worked for both us,” Phinney said. “Building trust took some time, but ultimately we reached a point where our colleagues and direct reports understood we could speak for one another on most issues, and we could quickly consult to provide answers whenever we needed to.”
Their model ultimately saved time because one could attend meetings to represent them both. Issues could be quickly addressed from both the clinical and business perspectives, and decisions made more quickly.
How to walk the talk
Improving physician satisfaction, loyalty and retention requires more than stating your commitment to engaging physicians and advanced practitioners in strategic decisions. MountainView Medical Group, Las Cruces, N.M., took a practical, data-driven approach to “walk the talk” of a physician-led/professionally managed organization.
A three step process — professionally facilitated into stages of discovery, team building and strategic planning — engaged clinicians with administrators in dyad teams, making strategic planning a “team sport” to:
- Develop the medical group’s mission, vision and core values.
- Identify and prioritize strategic objectives.
- Move forward together to achieve shared goals.
The initial discovery phase helps identify and break down the barriers to full and equal engagement. Then, team building helps bridge generational, gender and personality differences, ensuring that teams communicate effectively and stay focused on actionable goals. Using this best-practice approach, the practice ensured that all voices were heard so that strategic planning achieved alignment with the organization’s overall growth objectives.
Discovery: The value of objective, data-driven insight
 Everyone is familiar with the phrase that you don’t know what you don’t know. It makes sense to start the process by asking questions, listening closely and reporting transparently. Physicians, advanced practitioners and administrators know there are competing priorities and will be more likely to engage in a planning process in which decisions are based on data rather than a squeaky wheel or gut feel.
Everyone is familiar with the phrase that you don’t know what you don’t know. It makes sense to start the process by asking questions, listening closely and reporting transparently. Physicians, advanced practitioners and administrators know there are competing priorities and will be more likely to engage in a planning process in which decisions are based on data rather than a squeaky wheel or gut feel.
In the case of MountainView, a comprehensive survey incorporated inputs from the lead physician and administrator, along with an anonymous physician and manager engagement survey. The practice then did an overlay of national benchmark data.
Thus, MountainView could see evidence of the group’s solid foundation formed by positive relationships and mutual respect among colleagues for their competency. That meant that more focus could be placed on bridging operational gaps that were mutually identified. Using a scatter-plot matrix, the teams could see for themselves where there was consensus on areas of high importance that needed improvement, and therefore should become a priority.
Team building: Ensuring effective communication and outcomes
Leaders of any organization will attest to the challenge of keeping teams engaged when there is a highly diverse mix of work styles, generations, schedules and levels of experience.
The challenge of merging worlds at MountainView was significant. Due to rapid growth, only 37% of the providers had been with the group for more than three years. Another 37% had two or three years of tenure, and 26% had been with the group for one year or less. About three quarters had been individually recruited, while the other one quarter had joined through practice acquisition. Because the medical group had been formed through a combination of recruitment, mergers and acquisitions, there were several different organizational cultures and individual expectations that influenced the way providers worked and interacted.
Team building also was needed to bridge generations within the medical staff. Baby boomers represented 35% of the provider group, while 52% were members of Gen X. On the administrative side, only one member of the administrative team was a baby boomer, with the rest members of Gen X.
Finding common ground can seem daunting, but overlaying the demographic mix with Myers-Briggs indicators to better leverage differences and similarities helped to improve communication and optimize the team’s problem solving power.
Complementary strengths based on generation, gender and personality were maximized in ways relevant to MountainView’s strategic objectives. As the strategic planning phase began, “soft skills” represented within each team were identified to effectively move the ball down the field toward MountainView’s strategic goals.
Strategic Planning: Developing Shared Mission, Vision and Core Values
Based on the foundation built in the first two stages, MountainView avoided the common mistakes many organizations make when they set strategy in a vacuum, avoid tough questions or fail to examine long-held practices. The discovery and team-building phases provided a high level of trust that enabled the group to conduct the strengths, weaknesses, opportunities and threats (SWOT) analysis with clear eyes and equal measures of candor and respect. Leaders knew they could safely press each other for an honest assessment of strengths and weaknesses.
MountainView went beyond identifying weaknesses and questioned the areas of the practice that everyone assumed to be strengths. After developing the mission and vision as a group, MountainView then formed teams to own and articulate a core value and to tackle a specific business objective that had been prioritized. For example, the “excellence” core value team tackled the priority of timely onboarding in critical areas.
In this final phase, each team was ready to focus on actionable goals, solve barriers, build systems and schedules for accountability, create metrics and establish a communication plan for reporting progress.
Dyad teams work
Blending objective, data-driven insight with facilitated interaction, fresh thinking and exposure to best practices, the dyad teams fully engaged to tackle challenges and opportunities together. Key engagement indicators have increased. In the initial six month period, MountainView’s provider engagement “top box” score increased by 14%. In addition, the top box score for those who recommend the practice increased by 20%. Known as net promoters, this score is an indicator of overall satisfaction and loyalty.
MountainView is continuing to build on communication, trust and supportive working relationships to connect physicians to the organization and keep growing as a physician-led/professionally managed enterprise.
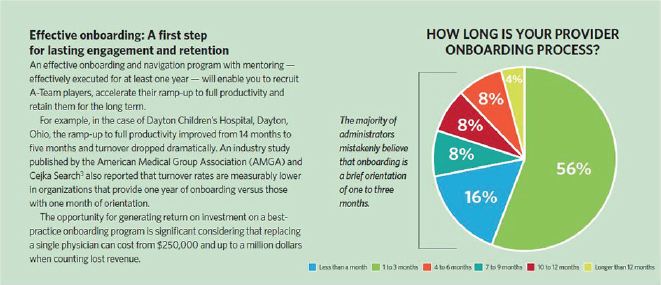
Note: American Medical Group Association. “Annual physician retention survey,” AMGA and Cejka Search, March 18, 2013.
Download a printable copy of the MGMA Connections article and the case study about the results we achieved with MountainView.
